The Zer0Now Campaign is proud to put our voice behind 16 days of activism. Brava to the fed gov for announcing in its #thronespeech intention to act on the important initiative we have been calling for. So needed! #16Days #orangetheworld #MeToo #OurActionsMatter pic.twitter.com/6s3a2qghl1
— Kathleen Finlay | 🇨🇦🇺🇸🇬🇧 (@ZeroHarmNow) December 8, 2019
Too many women and men, across cultures and societies, encounter sexual violence. It’s a global public health issue that increases people’s vulnerability to a host of physical, psychological and social difficulties. We must do something to implement best practice interventions and policies to prevent and address this widespread problem.
Joan Cook, PhD
Yale School of Psychiatry
A Call for a National Trauma-Informed Strategy to Raise Awareness of, and Increase Clinical Supports for, the Life-Threatening Physical and Emotional Health Impacts of Sexual Violence and its Frequently Harmful Aftermath
The sequelae of sexual violence often inflict emotional and physical harm long after the traumatic event. Much of it is caused by lack of trauma-informed awareness and misapprehension of the profound psychological and physical conditions that can arise in the post-trauma period. But much of the harm arises from the deliberate actions of organizations whose purpose is to punish or discredit the victim, often with the intent of silencing others who might come forward. The impact of these actions on a victim can devastate an entire remaining life. They can even be life-ending. We need to have zero tolerance for both situations. And we need it now.
 In 2010, 19-year-old college freshman Lizzy Seeberg killed herself after being sexually assaulted by a Notre Dame University football player. The aftermath and mishandling of the assault caused her to slip into a deep depression. Following Lizzy’s tragic passing, her family felt completely betrayed by the university’s inept and insensitive response, and by failures in the police investigation.
In 2010, 19-year-old college freshman Lizzy Seeberg killed herself after being sexually assaulted by a Notre Dame University football player. The aftermath and mishandling of the assault caused her to slip into a deep depression. Following Lizzy’s tragic passing, her family felt completely betrayed by the university’s inept and insensitive response, and by failures in the police investigation.
In 2013, Frances Andrade, an accomplished U.K. violinist, took a fatal overdose after learning the jury in the trial of the man who sexually abused her was instructed by the judge to find not guilty verdicts for several charges.
In 2018, former RCMP constable Krista Carle took her life after repeated incidents of sexual misconduct and emotional harm caused by the way the Force responded to her coming forward .
Sexual violence is one of the worst experiences any woman can face. So why are victims often hit by a second assault in the form of avoidable emotional harm inflicted by the officials and institutions we trust when we reach out for help?
 Every day, we see more shocking evidence of how sexual violence and sexual harassment are destroying careers and devastating lives. Too many who interact with victims, from healthcare professionals and HR staff to judges and heavy-handed lawyers, add to the toxic layers of emotional harms and adverse medical conditions faced by women who come forward. Most often, this results from a lack of trauma-informed understanding.
Every day, we see more shocking evidence of how sexual violence and sexual harassment are destroying careers and devastating lives. Too many who interact with victims, from healthcare professionals and HR staff to judges and heavy-handed lawyers, add to the toxic layers of emotional harms and adverse medical conditions faced by women who come forward. Most often, this results from a lack of trauma-informed understanding.
Our HealingNow™ initiative seeks to change this situation and make everyone more aware of the complex neurological and physiological sequelae of sexual violence and sexual harassment. It’s part of The Zer0Now Campaign’s™ effort to make real progress for everyday women in the workplace, in the community and on the campus.
Sexual violence, including threatening or aggressive forms of sexual harassment, is one of the most traumatic and humiliating experiences any woman can face. In addition to profoundly violating a victim’s dignity and fundamental human rights, it can produce a wide-range of detrimental emotional and physical health outcomes. Some can last for years, even decades. Some can be life-ending.
I know the profound toll this social scourge takes on its victims — especially the emotional and physical consequences it leaves. I hear it in their broken voices. I see it in their tear-soaked words. I am a victim,too.
Over the years, many women have reached out to The Zer0Now Campaign™ to share their ordeals involving sexual violence, sexual harassment and workplace bullying. They began to do this long before #MeToo’s arrival.
I know all too well the profound toll this social scourge takes on its victims at every level — especially the emotional and other medical consequences it leaves. I hear it in their broken voices. I see it in their tear-soaked words.
I know it because I am a victim, too.
A study published in the Journal of the American Medical Association (JAMA) in 2019 found:
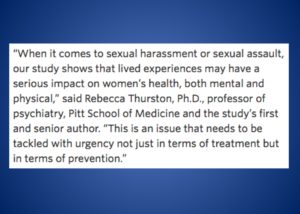
- Women in the study who reported prior sexual assault were three times more likely to experience depression and twice as likely to have elevated anxiety than women without a history of sexual trauma;
- Those who experienced either sexual assault or harassment were twice as likely to have sleep problems, including insomnia;
- Women who reported workplace sexual harassment had higher blood pressure than women who did not, at levels significant enough to put them at risk for stroke, aneurysms, kidney disease, heart attacks and other forms of heart disease;
- Sexual harassment was also linked to higher levels of triglycerides, a key risk factor for heart disease, which is the leading killer of women in the United States (and Canada).
Our call for a national strategy is intended to create a culture of trauma-informed healing among all those who interact with victims. One that avoids creating harm and helps with the process of recovery.
This is one of countless studies that confirm the shattering emotional and physical impact that sexual violence and threatening forms of sexual harassment have on victims.
Yet not all healthcare professionals are skilled in treating victims, or possess the necessary clinical information to make the right kind of assessment, according to experts. Some, by their cold demeanor and skeptical responses, fail to create a comfort level that enables already humiliated patients to share the full extent of their experience.
As acclaimed Yale psychologist Joan Cook, PhD, notes,
“Research on the prevalence and effects of trauma is large and growing. However, most health care professionals, such as psychologists, still only have a cursory knowledge of this science and little to no formal training in evidence-based psychosocial treatments for trauma-related disorders.” Dr. Cook, one of the world’s foremost authorities on sexual trauma in a recent op-ed called sexual violence a global public health issue that increases people’s vulnerability to a host of physical, psychological and social difficulties.
Toronto’s Women’s College Hospital echoes a similar view of the gaps in healthcare for women, including those arising from sexual violence.
“Half of all women in Canada have experienced at least one incident of physical or sexual violence since the age of 16, yet not all healthcare providers have the knowledge or skills to deliver sensitive care to these women.”

HealingNow™ was created in collaboration with The Center for Patient Protection’s Safer Women Health Initiative™ to raise awareness about the emotional and physical health risks associated with sexual violence and sexual harassment. An important part of our focus is on the harm caused by defective and ill-informed post-trauma responses and the need to combat the damage caused by what Jennifer Freyd, PhD, calls institutional betrayal.
Clinical work by Dr. Freyd in betrayal trauma theory led to the development of her concept of institutional betrayal. Her findings confirm that when a traumatic incident is followed by insensitive or abusive responses by trusted players like healthcare professionals, public institutions, government agencies, judges, private corporations or law enforcement authorities, the risk to a victim’s well-being rises sharply.
 Depression, anxiety, PTSD, self-harm and adverse physical outcomes are among the recognized sequelae of betrayal trauma identified by Dr. Freyd. The high-profile deaths by suicide involving 19-year-old college freshman Lizzy Seeberg, to which Dr. Freyd refers in her research, and former RCMP constable Krista Carle, which I have written about, are a vivid, and so heartbreaking, reminder of the catastrophic risks associated with institutional betrayal following sexual violence.
Depression, anxiety, PTSD, self-harm and adverse physical outcomes are among the recognized sequelae of betrayal trauma identified by Dr. Freyd. The high-profile deaths by suicide involving 19-year-old college freshman Lizzy Seeberg, to which Dr. Freyd refers in her research, and former RCMP constable Krista Carle, which I have written about, are a vivid, and so heartbreaking, reminder of the catastrophic risks associated with institutional betrayal following sexual violence.
We need to reimagine our approach to suicide prevention, which is now a healthcare crisis in some parts of society. The U.S. FCC has recommended adoption of a simple, easy to recall three digit number (988) to access the national suicide prevention lifeline. It has been shown to have the potential to save lives and it needs to be adopted in Canada, too.
In reaching out to The Zer0Now Campaign™ over the years, many woman have recounted being shocked, and harmed, by the insensitive and inadequate medical care they received. A general lack of trauma-informed awareness displayed during clinical visits, particularly at the primary physician level, was a disturbingly recurring theme. When women, and especially victims of sexual violence, do not have an adequate comfort zone and level of confidence in their interactions with healthcare professionals, they are less inclined to be fully candid.
Any barriers that contribute to a dysfunctional relationship or a breakdown in trust and communication in the healthcare setting are an open invitation to diagnostic errors and other risks. Poor communication between the patient and physician can raise the possibility of higher risk outcomes, especially when the use of antidepressant medication, like Effexor (venlafaxine), is introduced. An overdose of the drug Effexor is reported to have been the cause of Lizzy Seeberg’s death.
Another reported harm to victims caused by the healthcare system has been the use of the so-called independent medical examination (IME). These have been required by employers and health insurance carriers in certain situations where victims report post-trauma symptoms. The reality is that many IMEs are far from “independent.” It is not uncommon for such examinations to be the paid product of cash-and-carry doctors who make a profit center out of serving the interests of private companies, health insurance providers and law firms. This kind of rigged investigation can become a quick launching pad for institutional betrayal.
We need to create a culture of healing among all those who interact with victims, and especially among healthcare professionals, that avoids creating harm and helps with the process of recovery. It is important that primary care physicians acquaint themselves with the growing knowledge base of trauma-informed practices and begin to screen patients for possible sexual violence in the same way healthcare practices screen for smoking and other high-risk behaviour.
Victims, and their families, also need to become informed, early in the post-trauma period, of the complex range of emotional and medical issues that can confront them as they journey through this life-altering ordeal.
Policy makers and public authorities, including law enforcement agencies, need to gain a better understanding of the potential for serious emotional and medical reactions that can occur, especially when victims are confronted by insensitive or disbelieving words or actions or by situations that act to trigger harmful memories.
“It looks like the Canadian Senate’s actions could easily be viewed as a case of institutional betrayal in the eyes of the survivors.”
 The need for trauma-informed thinking on the part of judges was recognized by Canada’s parliament with the passage by the House of Commons of Bill C-337. The legislation would have required training of judges on the neurobiological dynamics of the traumatic sexual violence experience and its impact on the brain. The need is well documented in other jurisdictions. Outrageously, the bill died in the Senate and never became law. You can read my recent comments on that subject here.
The need for trauma-informed thinking on the part of judges was recognized by Canada’s parliament with the passage by the House of Commons of Bill C-337. The legislation would have required training of judges on the neurobiological dynamics of the traumatic sexual violence experience and its impact on the brain. The need is well documented in other jurisdictions. Outrageously, the bill died in the Senate and never became law. You can read my recent comments on that subject here.
In addition, the Senate has displayed staggering ineptitude and victim-betrayal in dealing with sexual misconduct in its own ranks. Victims have been re-traumatized by botched investigations, a lack of transparency, and the absence of anything even remotely connected with a trauma-informed approach to the issue. As Joan Cook, the Yale psychologist, told The Zer0Now Campaign™ in an exclusive interview: “Based on my understanding of what has been described to me, it looks like the Canadian Senate’s actions could easily be viewed as a case of institutional betrayal in the eyes of the survivors.”
Insensitivity and inappropriate remarks from the bench, which many experts interpret as an underlying ignorance of trauma-related facts that militate against a victim’s ability to recount events in a linear fashion — and which thereby distort reasonable judicial outcomes — are a recognized factor that prevents women from entering the doors of justice. No woman who has experienced sexual violence wants to be re-traumatized and turned into a victim all over again by a rigged or unfair system.
The media also has an important role in raising awareness about the longer-term dangers of sexual violence and related abuse. In particular, media outlets need to ensure that, in responding to victim outreach, journalists do not cause more damage and contribute to feelings of low self-worth or isolation through their insensitive actions or by ignoring these overtures altogether. It happens more often than most realize, and is often reflected in the stories victims share with Zer0Now.
Recently, The Globe and Mail focused on the victim trauma experienced by several women resulting from incidents of sexual abuse at the hands of a Toronto-based physician. The article made the point that not only did devastating harm occur during the incidents of sexual misconduct, but the emotional impact was magnified by the mishandling of the disciplinary process that is supposed to protect patients from harmful professional conduct.
When the quest for healing in a relationship of professional trust is broken, and perverted into an encounter with harm, the damage is particularly acute. Similar to the experience patients and families recount in the healthcare setting when dealing with the aftermath of medical errors, victims of sexual violence often say that the way the system handled their concerns after they came forward made the situation so much worse. That is the curse of institutional betrayal.
Leaving a victim worse off has no place in any process that purports to deal in a responsible fashion with women facing the most devastating time of their lives.
We need to view the emotional and physical conditions that can arise from sexual violence through the same urgent lens that decades ago made us see smoking as a contributor to physical harm and death. Without a doubt, sexual violence is hazardous to your health.
Our HealingNow initiative calls for the creation of a national strategy and awareness campaign to address, and reduce, the profound emotional and physical conditions that can arise from incidents of sexual violence, especially when they are mishandled. Only when there is a fuller understanding of the acute harms that are inflicted on victims can there be any hope that the actors who compound that harm, whether by ill-intention or by ineptitude, will change their ways.
Of course, many of the health-related impacts and characteristics of sexual violence, like those involving the neuroscience of trauma, are complex. But oftentimes adverse impacts can be mitigated, or even avoided altogether, by following the basic healing principles captured with these timeless virtues: Listen | Learn | Believe | Respect | Support. That’s not brain science. That’s just basic human contact, consideration and compassion. But it can make such a difference!
We believe that when it comes to the handling of sexual violence and related abuses, nothing less than a do no harm creed is acceptable. This applies not just to the medical profession — the traditional adherents to this ancient injunction — but to everyone else who has responsibility for interacting with and responding to victims who come forward, including bystanders and co-workers. Trauma-based practices need to inform and guide all those who hold a victim’s well-being in their hands.
Too much avoidable harm happens every day because of a lack of trauma-informed awareness and a fuller understanding of the extent to which all forms of sexual violence and their mishandling can be hazardous to a victim’s health, and sometimes life-threatening. We need to view the emotional and physical conditions that can arise from sexual violence in the same light as we saw smoking decades ago. Like smoking, the effects are traceable, harm-producing and life-altering. As in the case of smoking, these harms are largely avoidable, and the failure to properly recognize and treat them adds disproportionately to their risks.
Just as awareness of the risks associated with smoking was raised by public education efforts decades ago, understanding of the risks and sequelae of sexual violence by everyone, including healthcare professionals — and social disapproval of its causes — need to be elevated by public awareness.
Right now, the way too many victims are treated by institutions, the courts, employers and even by healthcare professionals, is the equivalent of having smoke blown directly into their faces. There is no excuse for this. It needs to change.
If you are a lawmaker, policy leader, scholar, healthcare professional and, especially, if you are a victim or survivor, and you would like to encourage or support our call for a national strategy, please contact me directly here.
Kathleen Finlay
Founder, The Zer0Now Campaign™
RELATED
Reimagine Life: A more innovative approach to suicide prevention
A Roadmap for the Government to Act Against Gender-based Violence
Stop Letting the System Assault Victims of Sexual Violence Over and Over
When Toxic Work Culture Adds to the Trauma of Sexual Misconduct
Stop Sexual Misconduct from Being Fatal
Sexual assault and harassment linked to long-term health problems for women
 About The Zer0Now Campaign™
About The Zer0Now Campaign™
The Zer0Now Campaign™ works to combat the conditions that lead to sexual violence and the harm of institutional betrayal. We champion changes in legislation and initiatives to make the workplace, the community and the campus safer. We work every day with victims in the everyday world to support them on their healing journey.
 About The Center for Patient Protection™
About The Center for Patient Protection™
The Center for Patient Protection™ works to improve patient safety and reduce medical harms in the hospital setting. We advocate for greater transparency to empower patients and families in their decisions, champion healing virtues like compassion and respect at all levels of care, and use patient experiences to assist providers in the delivery of safer outcomes. HealingNow™ is an outreach of The Center’s Safer Women’s Health Initiative™, which focuses on the unique healthcare needs of women, and gender-based barriers to obtaining it.
